The Science of Bedsores: What Causes Them
Are you or a loved one experiencing the pain and discomfort of bedsores?
Despite being a common condition, the science behind bedsores is still widely misunderstood. Bedsores, also known as pressure ulcers, are not just surface-level irritation. They are the result of a complex interaction between skin, muscle, and bone. The underlying causes of bedsores are rooted in the biomechanics of our bodies and the pressure exerted on certain areas of the skin. Let’s delve into the science behind bedsores, exploring the biological processes that lead to their development.
Skin Anatomy and Physiology
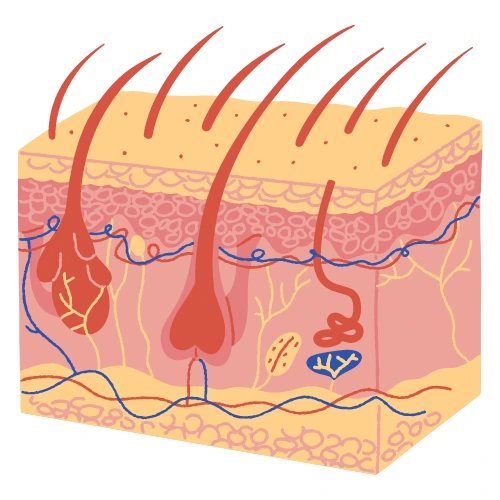
The skin is the largest organ of the body, serving as a protective barrier between the internal organs and the outside environment. It consists of three main layers: the epidermis, dermis, and subcutaneous tissue. The epidermis is the outermost layer and is responsible for providing protection from the environment. It also contains melanin, which gives skin its color.
The dermis is the middle layer and contains blood vessels, hair follicles, and sweat glands. It is responsible for providing nutrients and oxygen to the skin, as well as regulating body temperature. The subcutaneous tissue is the innermost layer and is primarily composed of fat. It serves as an energy store, insulation, and cushioning for the body.
The blood vessels in the skin play a vital role in maintaining skin health. They provide nutrients and oxygen to the skin cells, helping them to repair and regenerate. As we age, however, the blood vessels in the skin can become less efficient, leading to a decline in skin health.
The impact of aging on skin health is also evident in the thinning of the skin, loss of elasticity, and reduced collagen production. This can lead to a higher risk of developing bedsores, also known as pressure ulcers, which are areas of damaged skin caused by prolonged pressure on the skin.
Understanding the anatomy and physiology of the skin can help in preventing bedsores and promote overall skin health. By taking proactive measures to protect and care for the skin, we can maintain its integrity and prevent the development of painful and potentially life-threatening bedsores.
Pressure and Shear
When it comes to preventing bedsores, understanding pressure and shear is crucial. Pressure is the force exerted on the skin when the body is in contact with a surface, while shear refers to the sliding or rubbing of tissues against each other. The combination of pressure and shear can cause damage to the skin and underlying tissues, leading to the formation of bedsores.
The mechanics of pressure involve the compression of blood vessels, which limits blood flow and reduces the delivery of oxygen and nutrients to the tissues. This can lead to tissue damage and cell death, particularly in areas where there is already limited blood flow, such as bony prominences.
Shear forces, on the other hand, cause tissues to slide against each other, which can stretch and tear blood vessels and damage tissues. When pressure and shear are present at the same time, they can have a synergistic effect, increasing the risk of tissue damage.
To prevent bedsores, it is important to reduce pressure and shear on vulnerable areas of the body, such as the heels, hips, and sacrum. This can be achieved through regular repositioning, the use of specialized cushions and mattresses, and the use of proper lifting and transferring techniques.
By understanding the mechanics of pressure and shear, caregivers and healthcare providers can take proactive steps to prevent the development of bedsores and promote skin health.
The Stages of Bedsores

Bedsores are classified into four stages, each of which describes the severity of the ulcer and the extent of tissue damage:
Stage 1: Non-blanchable erythema
This is the earliest stage of bedsore, and it is characterized by redness and inflammation of the skin. The affected area may be warm to the touch and may feel firmer or softer than the surrounding skin. The skin may not blanch when pressed with a finger.
Stage 2: Partial thickness skin loss
At this stage, the ulcer has progressed to the point where there is damage to the outermost layer of skin, as well as the underlying tissue. The wound may look like a blister or an open sore, and there may be some drainage.
Stage 3: Full-thickness skin loss
In this stage, the ulcer has progressed even further, and there is no damage to the entire thickness of the skin. The wound may look like a deep crater, and there may be a significant amount of drainage.
Stage 4: Full-thickness skin and tissue loss
This is the most severe stage of bedsore, and it is characterized by extensive tissue damage, including damage to muscle, bone, and other underlying structures. The wound may be very deep and may expose tendons, muscles, or bones.
It is important to note that the severity of bedsore can progress quickly, and prompt treatment is essential to prevent further tissue damage and complications. Regular turning and repositioning of immobile patients, maintaining proper nutrition and hydration, and keeping the skin clean and dry can all help prevent the development of bedsores.
Risk Factors for Bedsores
Bedsores are a painful and potentially life-threatening condition that can develop in people who are bedridden or have limited mobility. There are several risk factors that increase the likelihood of developing bedsores, including age, chronic health conditions, immobility, and incontinence.
As we age, our skin becomes thinner and more fragile, which makes us more susceptible to bedsores. Chronic health conditions such as diabetes, cardiovascular disease, and obesity can also increase the risk of developing bedsores, as they can impair blood flow and compromise skin health.
Immobility is perhaps the most significant risk factor for bedsores, as it prevents blood flow to the affected area and puts pressure on the skin. This pressure can cause skin cells to die, leading to the development of bedsores.
Additionally, incontinence can also increase the risk of bedsores, as constant exposure to moisture can cause skin breakdown and increase the risk of infection.
It is important to be aware of these risk factors, especially if you or a loved one is bedridden or has limited mobility. By taking proactive measures to prevent bedsores, such as repositioning regularly, using special cushions, and keeping the skin clean and dry, you can reduce the risk of developing this painful and potentially life-threatening condition.
Diagnosing Bedsores
Diagnosing bedsores is a critical aspect of their treatment. The diagnosis typically involves a combination of physical examination, imaging tests, and laboratory tests.
During a physical examination, a healthcare professional will examine the affected area and assess the severity of the wound. They will look for signs of inflammation, redness, warmth, and drainage. They may also use a special tool to measure the size and depth of the wound.
Imaging tests, such as X-rays or MRI scans, may be used to determine the extent of tissue damage and whether there is an underlying bone or tissue infection. These tests can also help identify any other underlying medical conditions that may be contributing to the development of the bedsores.
Laboratory tests may also be ordered to help diagnose any underlying infections or medical conditions that may be contributing to the development of the bedsores. For example, a blood test may be done to check for signs of infection, such as an elevated white blood cell count.
Overall, a thorough and accurate diagnosis is crucial to developing an effective treatment plan for bedsores. If you suspect you or a loved one may have a bedsore, it is important to seek medical attention promptly to prevent the condition from worsening.
Complications of Bedsores
Bedsores can have serious complications if left untreated or poorly managed. One of the most common complications is an infection, which can occur when bacteria enter the open wound of the sore. The risk of infection is higher in individuals with weakened immune systems or poor circulation.
Sepsis is another potential complication of bedsores. Sepsis occurs when the body’s immune system overreacts to an infection, leading to widespread inflammation and organ damage. Sepsis is a medical emergency and requires immediate treatment.
Cellulitis is also a possible complication of bedsores. Cellulitis is a bacterial skin infection that can occur when bacteria enter the skin through a crack or wound. Symptoms of cellulitis include redness, swelling, warmth, and pain in the affected area. Cellulitis can be treated with antibiotics, but it is important to seek medical attention promptly to prevent the infection from spreading.
It is crucial to prevent and properly manage bedsores to avoid these and other complications. Regularly repositioning individuals who are bedridden or have limited mobility, maintaining good skin hygiene, and keeping the skin moisturized and protected can help prevent the development of bedsores.
Prognosis for Bedsores
The prognosis for bedsores depends on the stage of the sore, the individual’s overall health, and the effectiveness of treatment. In the advanced stages of bedsores, there can be extensive damage to the skin, tissues, and muscles. This can lead to chronic pain, reduced mobility, and impaired wound healing.
Furthermore, bedsores have a high rate of recurrence, making them difficult to manage. Prevention is key, and management strategies include frequent repositioning, proper nutrition, and the use of specialized support surfaces.
Effective management of bedsores is essential to prevent complications such as infection, sepsis, and cellulitis. These complications can be life-threatening, particularly in older adults and those with weakened immune systems. Regular monitoring and follow-up care are important to prevent complications and ensure optimal healing.
In conclusion, the prognosis for bedsores can vary depending on the individual and the stage of the sore. Effective management strategies can help prevent future bedsores and reduce the risk of complications. It is important to seek medical attention promptly if you or a loved one develops a pressure ulcer to ensure timely and effective treatment.
What does the research say?
This study by Dr. Wen Zhong looked at how bedsores are caused and how they can be prevented. Bedsores are a problem when people are in hospitals or nursing homes, especially older people. They are caused by pressure on the skin, which can be from things like clothing or bedding.
The study looked at a nursing home and asked about the residents’ skin problems and the type of clothes and bedding they used.
Moreover, they found that people who couldn’t move around much were more likely to get bed sores because their skin was in contact with the fabric for a long time. This study is important because it shows that the type of fabric people use can make a difference in preventing bedsores, especially for people who can’t move around much.
This study by Dr. Debashish Nayak says bedsores can be very expensive to treat and can even cause death. Despite being a common problem, there is still little research done to understand why bedsores occur.
There are two different theories about how they happen, but neither has been proven. Pressure, shear stress, and ischemia are thought to be involved, but it’s not fully understood.
There is not enough awareness about how to prevent or treat bedsores. There are some scales available to identify patients at high risk, with the Braden scale being the most widely accepted. Dressings and pressure relief devices are also available, but there is not enough research to determine which one is best.
Conclusion
Bedsores are a serious problem affecting a large number of patients worldwide. The science behind bedsores is complex and not fully understood, but it is clear that prevention and early intervention are crucial in avoiding complications.
Have you or someone you know experienced bedsores? What strategies have been effective in preventing or treating them? Share your thoughts and experiences in the comments below.

